Adipose Tissue Dysfunction in PCOS
DOI:
https://doi.org/10.18311/jer/2023/34082Keywords:
Adipocyte, Adiponectin, Adipose Tissue, Follicle Stimulating Hormone, Luteinizing Hormone, PCOSAbstract
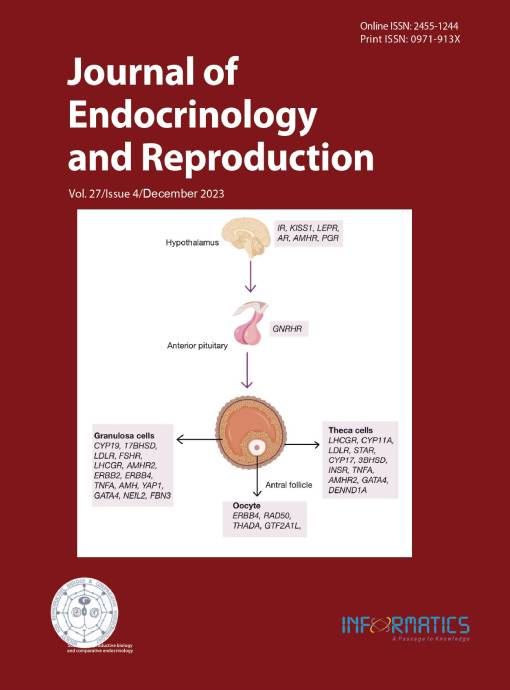
Polycystic Ovary Syndrome (PCOS) is one of the most common endocrine diseases among women of reproductive age; however, its aetiology is unclear. PCOS is linked to many metabolic manifestations and alterations such as obesity, insulin resistance, and cardiovascular diseases (CVD). Women with PCOS have intra-ovarian and systemic changes in their metabolite levels. Adipose tissue dysfunction plays a significant role in the pathophysiology of PCOS. Adipose tissue growth is disrupted by metabolic stress, leading to hypertrophy of adipocytes, which begin to express stress signals. Adipose tissue secretes autocrine and paracrine factors, called adipokines or adipocytokines. Adiponectin is an adipocyte-derived protein abundant in the bloodstream. Plasma adiponectin concentration is low in women with PCOS, obesity, CVD, and hypertension. Other adipocytokines with altered secretion in PCOS include leptin, resistin, apelin, visfatin, IL-6, IL-8, and TNF-α. Hormonal imbalance, untimely action of high LH, and consequent hyperandrogenism in women with PCOS may cause metabolic defects associated with adipose tissue dysfunction; however, there are no reports on the role of higher LH levels in adipose dysfunction and altered adipokine secretion. New medications with therapeutic potential have been developed that target adipokines for the treatment of PCOS. This review discusses the association between PCOS and altered adipokine production as a consequence of adipose dysfunction.
Downloads
Metrics
References
Kaur S, Ahamad I, Gouri Devi M, Singh R. Effect of body mass index on the biochemical outcome after fresh embryo transfer in women with and without Polycystic Ovary Syndrome (PCOS). J Pharmaceutical Negative Results (JPNR). 2021; 12(1):74-9.
Kaur S, Archer KJ, Devi MG, Kriplani A, Strauss JF 3rd, Singh R. Differential gene expression in granulosa cells from Polycystic Ovary Syndrome patients with and without insulin resistance: identification of susceptibility gene sets through network analysis. JCEM. 2012; 97:E2016-21. https://doi.org/10.1210/jc.2011-3441
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to Polycystic Ovary Syndrome. Fertil Steril. 2004; 81(1):19-25. https:// doi.org/10.1016/j.fertnstert.2003.10.004
Adashi EY, Cibula D, Peterson M, Azziz R. The polycystic ovary syndrome: the first 150 years of study. F S Rep. 2022; 4(1):2-18. https://doi.org/10.1016/j.xfre.2022.12.002
Singh R, Kaur S, Yadav S, Bhatia S. Gonadotropins as pharmacological agents in assisted reproductive technology and Polycystic Ovary Syndrome. Trends Endocrinol Metab. 2023; 34(4):194-215. https://doi.org/10.1016/j. tem.2023.02.002
Blank SK, McCartney CR, Helm KD, Marshall JC. Neuroendocrine effects of androgens in adult Polycystic Ovary Syndrome and female puberty. Semin Reprod Med. 2007; 25(5):352-9. https://doi.org/10.1055/s-2007-984741
Dumesic DA, Lobo RA. Cancer risk and PCOS. Steroids. 2013; 78(8):782-5. https://doi.org/10.1016/j.steroids.2013.04.004
Bedaiwy MA, Abdel-Rahman MY, Tan J, et al. Clinical, hormonal, and metabolic parameters in women with subclinical hypothyroidism and Polycystic Ovary Syndrome: A cross-sectional study. J Womens Health (Larchmt). 2018; 27(5):659-64. https://doi.org/10.1089/ jwh.2017.6584
Escobar-Morreale HF, San Millán JL. Abdominal adiposity and the Polycystic Ovary Syndrome. Trends Endocrinol Metab. 2007; 18(7):266-72. https://doi.org/10.1016/j. tem.2007.07.003
Diamanti-Kandarakis E, Dunaif A. Insulin resistance and the Polycystic Ovary Syndrome revisited: an update on mechanisms and implications. Endocr Rev. 2012; 33(6):981-1030. https://doi.org/10.1210/er.2011-1034
Fedeli V, Catizone A, Querqui A, Unfer V, Bizzarri M. The Role of Inositols in the hyperandrogenic phenotypes of PCOS: A re-reading of Larner’s results. Int J Mol Sci. 2023; 24(7):6296. https://doi.org/10.3390/ijms24076296
Urbanek M. The genetics of the Polycystic Ovary Syndrome. Nat Clin Pract Endocrinol Metab. 2007; 3(2):103-11. https://doi.org/10.1038/ncpendmet0400
Fahs D, Salloum D, Nasrallah M, Ghazeeri G. Polycystic Ovary Syndrome: pathophysiology and controversies in diagnosis. Diagnostics (Basel). 2023; 13(9):1559. https:// doi.org/10.3390/diagnostics13091559
Mannerås-Holm L, Leonhardt H, Kullberg J, et al. Adipose tissue has aberrant morphology and function in PCOS: enlarged adipocytes and low serum adiponectin, but not circulating sex steroids, are strongly associated with insulin resistance. J Clin Endocrinol Metab. 2011; 96(2):E304-11. https://doi.org/10.1210/jc.2010-1290
Omabe M, Elom S, Omabe KN. Emerging metabolomics biomarkers of Polycystic Ovarian Syndrome; targeting the master metabolic disrupters for diagnosis and treatment. Endocr Metab Immune Disord Drug Targets. 2018; 18(3):221-9. https://doi.org/10.2174/1871530318666 180122165415
Legro RS, Kunselman AR, Dunaif A. Prevalence and predictors of dyslipidemia in women with Polycystic Ovary Syndrome. Am J Med. 2001; 111(8):607-13. https://doi. org/10.1016/S0002-9343(01)00948-2
Yilmaz M, Biri A, Bukan N, et al. Levels of lipoprotein and homocysteine in non-obese and obese patients with Polycystic Ovary Syndrome. Gynecol Endocrinol. 2005; 20(5):258-63. https://doi.org/10.1080/09513590400027265
Chen MJ, Ho HN. Hepatic manifestations of women with Polycystic Ovary Syndrome. Best Pract Res Clin Obstet Gynaecol. 2016; 37:119-28. https://doi.org/10.1016/j. bpobgyn.2016.03.003
Chang E, Varghese M, Singer K. Gender and sex differences in adipose tissue. Curr Diab Rep. 2018; 18(9):69. https:// doi.org/10.1007/s11892-018-1031-3
Hausman DB, DiGirolamo M, Bartness TJ, Hausman GJ, Martin RJ. The biology of white adipocyte proliferation. Obes Rev. 2001; 2(4):239-54. https://doi. org/10.1046/j.1467-789X.2001.00042.x
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003; 112(12):1796-808. https://doi.org/10.1172/ JCI200319246
Kershaw EE, Flier JS. Adipose tissue is an endocrine organ. J Clin Endocrinol Metab. 2004; 89(6):2548-56. https://doi. org/10.1210/jc.2004-0395
Virtue S, Vidal-Puig A. Adipose tissue expandability, lipotoxicity and the metabolic syndrome--an allostatic perspective. Biochim Biophys Acta. 2010; 1801(3):338-49. https://doi.org/10.1016/j.bbalip.2009.12.006
Rutkowski JM, Stern JH, Scherer PE. The cell biology of fat expansion. J Cell Biol. 2015; 208(5):501-12. https://doi. org/10.1083/jcb.201409063
Benrick A, Chanclón B, et al. Adiponectin protects against the development of metabolic disturbances in a PCOS mouse model. Proc Natl Acad Sci USA. 2017; 114(34):E7187-96. https://doi.org/10.1073/pnas.1708854114
Brennan KM, Kroener LL, et al. Polycystic Ovary Syndrome: Impact of lipotoxicity on metabolic and reproductive health. Obstet Gynecol Surv. 2019; 74(4):223-31. https:// doi.org/10.1097/OGX.0000000000000661
Dumesic DA, Phan JD, et al. Adipose insulin resistance in normal-weight women with Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2019; 104(6):2171-83. https://doi. org/10.1210/jc.2018-02086
Scheja L, Heeren J. The endocrine function of adipose tissues in health and cardiometabolic disease. Nat Rev Endocrinol. 2019; 15(9):507-24. https://doi.org/10.1038/ s41574-019-0230-6
Würfel M, Blüher M, Stumvoll M,et al. Adipokines as clinically relevant therapeutic targets in obesity. Biomedicines. 2023; 11(5):1427. https://doi.org/10.3390/biomedicines11051427
Steppan CM, Bailey ST, Bhat S, et al. The hormone resistin links obesity to diabetes. Nature. 2001; 409(6818):307-12. https://doi.org/10.1038/35053000
Lee YH, Pratley RE. The evolving role of inflammation in obesity and the metabolic syndrome. Curr Diab Rep. 2005; 5(1):70-5. https://doi.org/10.1007/s11892-005-0071-7
Haczeyni F, Bell-Anderson KS, Farrell GC. Causes and mechanisms of adipocyte enlargement and adipose expansion. Obes Rev. 2018; 19(3):406-20. https://doi. org/10.1111/obr.12646
Fain JN, Bahouth SW, Madan AK. TNFalpha release by the nonfat cells of human adipose tissue. Int J Obes Relat Metab Disord. 2004; 28(4):616-22. https://doi.org/10.1038/ sj.ijo.0802594
Sayin NC, Gücer F, Balkanli-Kaplan P, et al. Elevated serum TNF-alpha levels in normal-weight women with polycystic ovaries or Polycystic Ovary Syndrome. J Reprod Med. 2003; 48(3):165-70.
Amato G, Conte M, Mazziotti G, et al. Serum and follicular fluid cytokines in Polycystic Ovary Syndrome during stimulated cycles. Obstet Gynecol. 2003; 101(6):1177-82. https://doi.org/10.1097/00006250-200306000-00009
Arner E, Westermark PO, Spalding KL, et al. Adipocyte turnover: relevance to human adipose tissue morphology. Diabetes. 2010; 59(1):105-9. https://doi. org/10.2337/db09-0942
Faulds G, Rydén M, Ek I, Wahrenberg H, Arner P. Mechanisms behind lipolytic catecholamine resistance of subcutaneous fat cells in the Polycystic Ovarian Syndrome. J Clin Endocrinol Metab. 2003; 88(5):2269-73. https://doi. org/10.1210/jc.2002-021573
Herman R, Kravos NA, Jensterle M, Janež A, Dolžan V. Metformin and insulin resistance: A review of the underlying mechanisms behind changes in GLUT4- mediated glucose transport. Int J Mol Sci. 2022; 23(3):1264. https://doi.org/10.3390/ijms23031264
Chang W, Goodarzi MO, Williams H, Magoffin DA, Pall M, Azziz R. Adipocytes from women with Polycystic Ovary Syndrome demonstrate altered phosphorylation and activity of glycogen synthase kinase 3. Fertil Steril. 2008; 90(6):2291- 7. https://doi.org/10.1016/j.fertnstert.2007.10.025
Corbould A, Dunaif A. The adipose cell lineage is not intrinsically insulin-resistant in Polycystic Ovary Syndrome. Metabolism. 2007; 56(5):716-22. https://doi. org/10.1016/j.metabol.2006.12.021
Villa J, Pratley RE. Adipose tissue dysfunction in Polycystic Ovary Syndrome. Curr Diab Rep. 2011; 11(3):179-84. https://doi.org/10.1007/s11892-011-0189-8
Weyer C, Foley JE, Bogardus C, Tataranni PA, Pratley RE. Enlarged subcutaneous abdominal adipocyte size, but not obesity itself, predicts type II diabetes independent of insulin resistance. Diabetologia. 2000; 43(12):1498- 506. https://doi.org/10.1007/s001250051560
Diamanti-Kandarakis E, Papavassiliou AG, Kandarakis SA, Chrousos GP. Pathophysiology and types of dyslipidemia in PCOS. Trends Endocrinol Metab. 2007; 18(7):280-5. https://doi.org/10.1016/j.tem.2007.07.004
Seow KM, Tsai YL, Hwang JL, Hsu WY, Ho LT, Juan CC. Omental adipose tissue overexpression of fatty acid transporter CD36 and decreased expression of hormonesensitive lipase in insulin-resistant women with Polycystic Ovary Syndrome. Hum Reprod. 2009; 24(8):1982-8. https:// doi.org/10.1093/humrep/dep122
Glintborg D, Højlund K, Andersen M, Henriksen JE, BeckNielsen H, Handberg A. Soluble CD36 and risk markers of insulin resistance and atherosclerosis are elevated in Polycystic Ovary Syndrome and significantly reduced during pioglitazone treatment. Diabetes Care. 2008; 31(2):328-34. https://doi.org/10.2337/dc07-1424
Fernández-Sánchez A, Madrigal-Santillán E, Bautista M, et al. Inflammation, oxidative stress, and obesity. Int J Mol Sci. 2011; 12(5):3117-32. https://doi.org/10.3390/ijms12053117
Cortón M, Botella-Carretero JI, Benguría A, et al. Differential gene expression profile in omental adipose tissue in women with Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2007; 92(1):328-37. https://doi. org/10.1210/jc.2006-1665
Echiburú B, Pérez-Bravo F, Galgani JE, et al. Enlarged adipocytes in subcutaneous adipose tissue associated with hyperandrogenism and visceral adipose tissue volume in women with Polycystic Ovary Syndrome. Steroids. 2018; 130:15-21. https://doi.org/10.1016/j.steroids.2017.12.009
Nohara K, Liu S, Meyers MS, et al. Developmental androgen excess disrupts reproduction and energy homeostasis in adult male mice. J Endocrinol. 2013; 219(3):259-68. https:// doi.org/10.1530/JOE-13-0230
Mannerås L, Cajander S, Holmäng A, et al. A new rat model exhibiting both ovarian and metabolic characteristics of Polycystic Ovary Syndrome. Endocrinology. 2007; 148(8):3781-91. https://doi.org/10.1210/en.2007-0168
Perello M, Castrogiovanni D, Giovambattista A, Gaillard RC, Spinedi E. Impairment in insulin sensitivity after early androgenization in the post-pubertal female rat. Life Sci. 2007; 80(19):1792-8. https://doi.org/10.1016/j.lfs.2007.02.013
Puttabyatappa M, Lu C, Martin JD, Chazenbalk G, Dumesic D, Padmanabhan V. Developmental programming: impact of prenatal testosterone excess on steroidal machinery and cell differentiation markers in visceral adipocytes of female sheep. Reprod Sci. 2018; 25(7):1010-23. https://doi. org/10.1177/1933719117746767
Keller E, Chazenbalk GD, Aguilera P, et al. Impaired preadipocyte differentiation into adipocytes in subcutaneous abdominal adipose of PCOS-like female rhesus monkeys. Endocrinology. 2014; 155(7):2696-703. https://doi.org/10.1210/en.2014-1050
Gupta V, Bhasin S, Guo W, et al. Effects of dihydrotestosterone on differentiation and proliferation of human mesenchymal stem cells and preadipocytes. Mol Cell Endocrinol. 2008; 296(1-2):32-40. https://doi.org/10.1016/j.mce.2008.08.019
Frayn KN, Karpe F, Fielding BA, Macdonald IA, Coppack SW. Integrative physiology of human adipose tissue. Int J Obes Relat Metab Disord. 2003; 27(8):875-88. https://doi. org/10.1038/sj.ijo.0802326
Luo L, Liu M. Adiponectin: friend or foe in obesity and inflammation. Med Rev (Berl). 2022; 2(4):349-62. https:// doi.org/10.1515/mr-2022-0002
Atzmon G, Pollin TI, Crandall J, et al. Adiponectin levels and genotype: a potential regulator of life span in humans. J Gerontol A Biol Sci Med Sci. 2008; 63(5):447-53. https:// doi.org/10.1093/gerona/63.5.447
Combs TP, Berg AH, Rajala MW, et al. Sexual differentiation, pregnancy, calorie restriction, and aging affect the adipocytespecific secretory protein adiponectin. Diabetes. 2003; 52(2):268-76. https://doi.org/10.2337/diabetes.52.2.268
Vionnet N, Hani EH, Dupont S, et al. Genomewide search for type 2 diabetes-susceptibility genes in French whites: evidence for a novel susceptibility locus for early-onset diabetes on chromosome 3q27-qter and independent replication of a type 2-diabetes locus on chromosome 1q21-q24. Am J Hum Genet. 2000; 67(6):1470-80. https:// doi.org/10.1086/316887
Kissebah AH, Sonnenberg GE, Myklebust J, et al. Quantitative trait loci on chromosomes 3 and 17 influence phenotypes of the metabolic syndrome. Proc Natl Acad Sci U S A. 2000;97(26):14478-14483. https://doi.org/10.1073/ pnas.97.26.14478
Fruebis J, Tsao TS, Javorschi S, et al. A proteolytic cleavage product of 30-kDa adipocyte complement-related protein increases fatty acid oxidation in muscle and causes weight loss in mice. Proc Natl Acad Sci USA. 2001; 98(4):2005-10. https://doi.org/10.1073/pnas.98.4.2005
Combs TP, Berg AH, Obici S, Scherer PE, Rossetti L. Endogenous glucose production is inhibited by the adipose-derived protein Acrp30. J Clin Invest. 2001; 108(12):1875-81. https://doi.org/10.1172/JCI14120
Yamamoto Y, Hirose H, Saito I, et al. Correlation of the adipocyte-derived protein adiponectin with insulin resistance index and serum high-density lipoproteincholesterol, independent of body mass index, in the Japanese population. Clin Sci (Lond). 2002; 103(2):137-42. https://doi.org/10.1042/cs1030137
Kubota N, Terauchi Y, Yamauchi T, et al. Disruption of adiponectin causes insulin resistance and neointimal formation. J Biol Chem. 2002; 277(29):25863-6. https://doi. org/10.1074/jbc.C200251200
Yamauchi T, Kamon J, Waki H, et al. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med. 2001; 7(8):941- 6. https://doi.org/10.1038/90984
Hotta K, Funahashi T, Arita Y, et al. Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Arterioscler Thromb Vasc Biol. 2000; 20(6):1595-9. https://doi.org/10.1161/01.ATV.20.6.1595
Matsubara M, Maruoka S, Katayose S. Decreased plasma adiponectin concentrations in women with dyslipidemia. J Clin Endocrinol Metab. 2002; 87(6):2764-9. https://doi. org/10.1210/jcem.87.6.8550
Sun W, Liu G, Liu B. Association between circulating adiponectin and heart rate recovery in women with Polycystic Ovarian Syndrome. Endocr Res. 2022; 47(2):56- 63. https://doi.org/10.1080/07435800.2021.2011908
Spritzer PM, Lecke SB, Satler F, Morsch DM. Adipose tissue dysfunction, adipokines, and low-grade chronic inflammation in Polycystic Ovary Syndrome. Reproduction. 2015; 149(5):R219-27. https://doi.org/10.1530/REP-14- 0435
Toulis KA, Goulis DG, Farmakiotis D, et al. Adiponectin levels in women with Polycystic Ovary Syndrome: a systematic review and a meta-analysis. Hum Reprod Update. 2009; 15(3):297-307. https://doi.org/10.1093/ humupd/dmp006
Zhang N, Shi YH, Hao CF, et al. Association of +45G15G(T/G) and +276(G/T) polymorphisms in the ADIPOQ gene with Polycystic Ovary Syndrome among Han Chinese women. Eur J Endocrinol. 2008; 158(2):255- 60. https://doi.org/10.1530/EJE-07-0576
Glintborg D, Frystyk J, Højlund K, et al. Total and High Molecular Weight (HMW) adiponectin levels and measures of glucose and lipid metabolism following pioglitazone treatment in a randomized placebo-controlled study in Polycystic Ovary Syndrome. Clin Endocrinol (Oxf). 2008; 68(2):165-74. https://doi.org/10.1111/j.1365- 2265.2007.03015.x
Glintborg D. Endocrine and metabolic characteristics in Polycystic Ovary Syndrome. Dan Med J. 2016; 63(4):B5232.
Vatannejad A, Kheirollahi A. Adiponectin/leptin and HOMA/adiponectin ratios in Iranian women with Polycystic Ovary Syndrome. Ir J Med Sci. 2023; 192(4):1793- 9. https://doi.org/10.1007/s11845-023-03408-4
Mishra P, Mittal P, Rani A, Bharti R, Agarwal V, Suri J. Adiponectin to leptin ratio and its association with insulin resistance in women with Polycystic Ovarian Syndrome. Indian J Endocrinol Metab. 2022; 26(3):239-44. https://doi.org/10.4103/ijem.ijem_137_22
Nishizawa H, Shimomura I, Kishida K, et al. Androgens decrease plasma adiponectin, an insulin-sensitizing adipocyte-derived protein. Diabetes. 2002; 51(9):2734-41. https://doi.org/10.2337/diabetes.51.9.2734
Panidis D, Kourtis A, Farmakiotis D, Mouslech T, Rousso D, Koliakos G. Serum adiponectin levels in women with polycystic ovary syndrome. Hum Reprod. 2003; 18(9):1790- 6. https://doi.org/10.1093/humrep/deg353
Dos Santos E, Dieudonné MN, Leneveu MC, Pecquery R, Serazin V, Giudicelli Y. In vitro effects of chorionic gonadotropin hormone on human adipose development. J Endocrinol. 2007; 194(2):313-25. https://doi.org/10.1677/ JOE-06-0101
Mannerås-Holm L, Benrick A, Stener-Victorin E. Gene expression in subcutaneous adipose tissue differs in women with Polycystic Ovary Syndrome and controls matched pair-wise for age, body weight, and body mass index. Adipocyte. 2014; 3(3):190-6. https://doi. org/10.4161/adip.28731
Asterholm IW, Scherer PE. Enhanced metabolic flexibility is associated with elevated adiponectin levels. Am J Pathol. 2010; 176(3):1364-76. https://doi.org/10.2353/ ajpath.2010.090647
Mahde A, Shaker M, Al-Mashhadani Z. Study of Omentin1 and other adipokines and hormones in PCOS patients. Oman Med J. 2009; 24(2):108-18.
Ravishankar Ram M, Sundararaman PG, Mahadevan S, Malathi R. Cytokines and leptin correlation in patients with Polycystic Ovary Syndrome: Biochemical evaluation in south Indian population. Reprod Med Biol. 2005; 4(4):247- 54. https://doi.org/10.1111/j.1447-0578.2005.00114.x
Franik G, Sadlocha M, Madej P, et al. Circulating omentin-1 levels and inflammation in Polycystic Ovary Syndrome. Ginekol Pol. 2020; 91(6):308-12. https://doi. org/10.5603/GP.2020.0057
Lee MW, Lee M, Oh KJ. Adipose tissue-derived signatures for obesity and type 2 diabetes: adipokines, cytokines, and MicroRNAs. J Clin Med. 2019; 8(6):854. https://doi. org/10.3390/jcm8060854
Dravecká I, Figurová J, Lazúrová I. Is Apelin a new biomarker in patients with Polycystic Ovary Syndrome? Physiol Res. 2021; 70(4):S635-41. https://doi.org/10.33549// physiolres.934708 86. Gao Y, Xin C, Fan H, Sun X, Wang H. Circulating apelin and chemerin levels in patients with Polycystic Ovary Syndrome: A meta-analysis. Front Endocrinol (Lausanne). 2023; 13:1076951. https://doi.org/10.3389/ fendo.2022.1076951
Jia J, Bai J, Liu Y, et al. Association between retinol-binding protein 4 and Polycystic Ovary Syndrome: A metaanalysis. Endocr J. 2014; 61(10):995-1002. https://doi. org/10.1507/endocrj.EJ14-0186
Chen P, Jia R, Liu Y, Cao M, Zhou L, Zhao Z. Progress of adipokines in the female reproductive system: A focus on Polycystic Ovary Syndrome. Front Endocrinol (Lausanne). 2022; 13:881684. https://doi.org/10.3389/ fendo.2022.881684
Nambiar V, Vijesh VV, Lakshmanan P, Sukumaran S, Suganthi R. Association of adiponectin and resistin gene polymorphisms in South Indian women with Polycystic Ovary Syndrome. Eur J Obstet Gynecol Reprod Biol. 2016; 200:82-8. https://doi.org/10.1016/j. ejogrb.2016.02.031
Tumu VR, Govatati S, Guruvaiah P, Deenadayal M, Shivaji S, Bhanoori M. An interleukin-6 gene promoter polymorphism is associated with Polycystic Ovary Syndrome in South Indian women. J Assist Reprod Genet. 2013; 30(12):1541-6. https://doi.org/10.1007/s10815-013-0111-1
Bril F, Ezeh U, Amiri M, et al. Adipose tissue dysfunction in Polycystic Ovary Syndrome. J Clin Endocrinol Metab. 2023; dgad356. https://doi.org/10.1210/clinem/dgad356
Xu Y, Zhu H, Li W,et al. Targeting adipokines in Polycystic Ovary Syndrome and related metabolic disorders: from experimental insights to clinical studies. Pharmacol Ther. 2022; 240:108284. https://doi.org/10.1016/j.pharmthera.2022.108284
 Ananya Aparupa
Ananya Aparupa